
| Ultra-sensitive Beta Nerve Growth Factor (NGF) ELISA Kit | |
Alternative name:
|
|
|
|
|
Nerve growth factor gene therapy using adeno-associated viral vectors prevents cardiomyopathy in type 1 diabetic mice |
|
| Diabetes is a cause of cardiac dysfunction, reduced myocardial perfusion, and ultimately heart failure. Nerve growth factor (NGF) exerts protective effects on the cardiovascular system. This study investigated whether NGF gene transfer can prevent diabetic cardiomyopathy in mice. We worked with mice with streptozotocin-induced type 1 diabetes and with nondiabetic control mice. After having established that diabetes reduces cardiac NGF mRNA expression, we tested NGF gene therapies with adeno-associated viral vectors (AAVs) for the capacity to protect the diabetic mouse heart. To this aim, after 2 weeks of diabetes, cardiac expression of human NGF or β-Gal (control) genes was induced by either intramyocardial injection of AAV serotype 2 (AAV2) or systemic delivery of AAV serotype 9 (AAV9). Nondiabetic mice were given AAV2-β-Gal or AAV9-β-Gal. We found that the diabetic mice receiving NGF gene transfer via either AAV2 or AAV9 were spared the progressive deterioration of cardiac function and left ventricular chamber dilatation observed in β-Gal-injected diabetic mice. Moreover, they were additionally protected from myocardial microvascular rarefaction, hypoperfusion, increased deposition of interstitial fibrosis, and increased apoptosis of endothelial cells and cardiomyocytes, which afflicted the β-Gal-injected diabetic control mice. Our data suggest therapeutic potential of NGF for the prevention of cardiomyopathy in diabetic subjects. | |
| Meloni M, et al. Diabetes. 2012 Jan;61(1):229-40. | |
Diabetes as a risk factor for Alzheimer's disease: insulin signalling impairment in the brain as an alternative model of Alzheimer's disease |
|
| Surprisingly little is known about the mechanisms that trigger the onset of AD (Alzheimer's disease) in sporadic forms. A number of risk factors have been identified that may shed light on the mechanisms that may trigger or facilitate the development of AD. Recently, T2DM (Type 2 diabetes mellitus) has been identified as a risk factor for AD. A common observation for both conditions is the desensitization of insulin receptors in the brain. Insulin acts as a growth factor in the brain and is neuroprotective, activates dendritic sprouting, regeneration and stem cell proliferation. The impairment of this important growth factor signal may facilitate the development of AD. Insulin as well as other growth factors have shown neuroprotective properties in preclinical and clinical trials. Several drugs have been developed to treat T2DM, which re-sensitize insulin receptors and may be of use to prevent neurodegenerative processes in the brain. In particular, the incretins GLP-1 (glucagon-like peptide-1) and GIP (glucose-dependent insolinotropic polypeptide) are hormones that re-sensitize insulin signalling. Incretins also have similar growth-factor-like properties as insulin and are neuroprotective. In mouse models of AD, GLP-1 receptor agonists reduce amyloid plaque formation, reduce the inflammation response in the brain, protect neurons from oxidative stress, induce neurite outgrowth, and protect synaptic plasticity and memory formation from the detrimental effects caused by β-amyloid production and inflammation. Other growth factors such as BDNF (brain-derived neurotrophic factor), NGF (nerve growth factor) or IGF-1 (insulin-like growth factor 1) also have shown a range of neuroprotective properties in preclinical studies. These results show that these growth factors activate similar cell signalling mechanisms that are protective and regenerative, and suggest that the initial process that may trigger the cascade of neurodegenerative events in AD could be the impairment of growth factor signalling such as early insulin receptor desensitization. | |
| Hölscher C. Biochem Soc Trans. 2011 Aug;39(4):891-7. | |
A study of serum concentrations and dermal levels of NGF in atopic dermatitis and healthy subjects |
|
| Nerve growth factor (NGF) was reported to be increased in the serum and skin of atopic dermatitis (AD) patients, to the extent that serum nerve growth factor levels were proposed to serve as a marker of disease severity. We studied NGF levels in the serum and dermis using skin microdialysis and attempted to correlate them with disease severity. We also examined if potential differences between morning and evening levels of NGF can explain the phenomenon of nocturnal itch. In addition, neurogenic inflammation and itch were induced using histamine iontophoresis in lesional and non-lesional skin and the effect of experimental itch on dermal NGF concentration was examined. We found that systemic (serum) and eczematous skin levels of NGF in AD are significantly lower in comparison to healthy controls. Serum NGF decreases from morning to late afternoon in both groups. Interestingly, serum NGF levels were correlated to disease severity in the morning in AD, although the NGF concentration in AD were significantly lower than in the healthy group. The local itch and neurogenic inflammation induction via experimental histamine reduced local NGF levels in the eczema and non-lesional skin in atopics, but not in the healthy controls, where it was slightly increased. The higher the clinical severity of the eczema, a significantly less pronounced effect of neurogenic inflammation on the local levels of NGF was found. The availability of measurable NGF might be reduced by a higher expression of NGF receptors. The fluctuations of NGF levels during the day suggest a complex modulation of this neurotrophin, potentially linked to stress or to an altered neurophysiological mechanism. | |
Papoiu AD et
al. Neuropeptides. 2011 Dec;45(6):417-22. Epub 2011 Sep 3. |
|
Increased cutaneous NGF and CGRP-labelled trkA-positive intra-epidermal nerve fibres in rat diabetic skin |
|
| In this study we have determined the amount of Nerve Growth Factor (NGF) and the innervation density of the glabrous hindpaw skin of diabetic rats (n=4) and controls (n=3). The proportion of intra-epidermal nerve fibres (IENF) expressing the high affinity NGF receptor (trkA) and calcitonin gene-related peptide (CGRP) were also determined. Four weeks after induction of diabetes by intraperitoneal streptozotocin injection skin was analyzed for: (i) NGF content using ELISA and (ii) the innervation density of peptidergic afferents that also expressed trkA using immunocytochemistry. NGF levels were approximately three-fold higher in diabetic skin compared to controls (diabetic: 134.7±24.0 (SD) pgml(-1), control: 42.7±21.5pgml(-1), p=0.002). As expected there was a significant reduction in IENF density in diabetic skin (2.7±1.3 fibresmm(-1)) compared to controls (6.9±1.5 fibresmm(-1); p=0.01). In diabetic rats there was no significant difference in the proportion of trkA-labelled IENF (diabetic 74±21%; control 83±15%, p=0.6), but significantly more trkA-positive IENF were also labelled by CGRP antibodies in diabetic skin compared to controls (diabetic 89±22%; control 38±2%, p=0.03). These data suggest that in diabetes the upregulation of cutaneous NGF may 'over-troph' the surviving axons, increasing CGRP labelling, which may be important in the aetiology of painful diabetic neuropathy. | |
| Evans L et al. Neurosci Lett. 2012 Jan 6;506(1):59-63. Epub 2011 Oct 25. | |
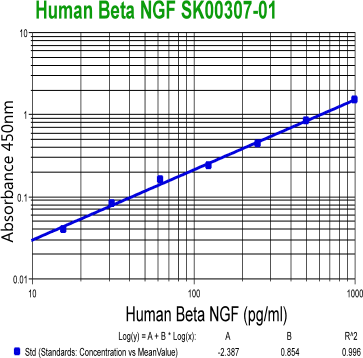 |
Beta NGF
(Human) ELISA Kit Code No.: SK00307-01 Size: 100 ug Price: $360.00 USD Standard range: 15.6 -1000 pg/ml Sensitivity: 7 pg/ml Sample Type: serum and plasma Intra-CV: 4-6% Inter-CV: 8-12% Data Sheet: PDF |
| Ultra-sensitive Beta NGF
(Human) ELISA Kit Code No.: SK00307-02 Size: 100 ug Price: $390.00 USD Standard range: 3.12 -200 pg/ml Sensitivity: 1 pg/ml Sample Type: serum and plasma Intra-CV: 4-6% Inter-CV: 8-12% Data Sheet: PDF |
|
|
|
| Name | Code No. |
Size |
Price ($) |
| Beta NGF (Human) ELISA Kit | SK00307-01 | 96 T | 360.00 |
| Ultra-sensitive Beta NGF (Human) ELISA Kit | SK00307-02 | 96 T | 390.00 |
|